January 4, 2015
This is the final installment of a three part series, ‘Chromatin as a Cancer Target.’ If you haven’t already, you can get up to speed here: Part I (Chromatin Writers) and Part II (Chromatin Erasers).
Therapeutic targeting of Chromatin Readers is an emerging area of drug discovery that has been gaining momentum in recent years, with most of the excitement stemming from therapeutic applications in oncology. Up until 2014, interest in this field was mostly reserved for academics, save a few small start-ups. However, in 2014 the biopharmaceutical industry began to take notice: in April Medivation inked a pre-clinical licensing deal from a small Michigan-based start-up, and more recently Merck opted to acquire a a Swiss biotech for a clinical-stage asset. More on these deals below, but first, the science…

As the nomenclature would imply, Chromatin Readers function in the recognition of covalent DNA and protein modifications. By ‘reading,’ Readers act to determine the functional outcome of post-translational modifications via the recruitment of additional protein complexes. Recall from the two previous Oncology Discovery posts that histone modifications are in constant flux via the activity of Chromatin Writers and Erasers. Chromatin Readers comprise a set of structurally diverse proteins. By definition, these proteins contain one or more protein domains, or modules, which read covalent modifications. Chromatin Readers come in many flavors with a variety of one or more different reader modules in a single protein. The following discussion will revolve around Readers of the bromodomain variety. Bromodomains are protein modules, which read acetyl lysine residues. Encoded within the human proteome are 61 distinct bromodomain modules; these modules are present within 46 unique proteins. Structure-based phylogeny of the human bromodomain family is pictured in Figure 1, and depicts eight major classes of bromodomain-containing proteins; distinct classes are based on structural similarities.

Of the eight distinct human bromodomain-containing protein classes, the bromodomain and extra-terminal (BET) class comprised of BRD2, BRD3, BRD4 and BRDT have received special attention. The domain architecture of these proteins is depicted in Figure 2. BET proteins contain conserved tandem N-terminal bromodomains (BD1 and BD2), which allow for interaction with acetylated histones and various nuclear proteins. By mediating interactions with acetylated chromatin, BD1 and BD2 allow for discrete localization of BET proteins at various chromosomal locations. In turn, BET proteins recruit regulatory complexes to influence gene expression. Of BET family members, the function of BRD4 has been most thoroughly studied and will be the primary subject of the following discussion. BRD4 regulates RNA-pol II-mediated elongation and transcription by directly interacting with the Mediator complex and pTEFb. Additionally, recent literature has shown direct BRD4 interactions with transcription factors, including NF-κB, ERα, p53, TWIST, and GATA-1, across a range of cancer types. These interactions occur via bromodomain-dependent and -independent mechanisms. Thus, in a cancer context-specific manner, BRD4 serves as a node between disease-relevant transcription factors and the transcriptional machinery. At enhancer and promoter regions, the combinatorial interactions among acetylated histones, transcription factors, nuclear proteins, and the transcriptional machinery allow BRD4 to mediate translation of the epigenetic code into RNA synthesis (Figure 2).


The first evidence demonstrating a role for BRD4 in cancer came from the identification of chromosomal translocations involving BRD4. Namely, the identification of NUT midline carcinoma (NMC), an aggressive epithelial malignancy, gave a genetically-linked line-of-sight for targeting BRD4 in cancer. In NMC patients chromosomal translocations give rise to in-frame BRD4 fusions with the NUT gene1. The BRD4-NUT fusion protein mediates an aberrant oncogenic transcriptional program, thus making it an ideal target for BRD4 inhibition. Indeed, the first well characterized BRD4 chemical probes, JQ1 and I-BET2,3, have shown marked (pre-clinical) activity in a wide range of cancers including NMC. By directly competing with acetylated lysine, JQ1 and I-BET engage BET bromodomains, resulting in the displacement of BRD4 from chromatin, and the disruption of BRD4-mediated transcriptional co-activation.
Pre-clinical studies
Since the structure of JQ1 was reported in a landmark Nature paper in 20102, the body of academic literature related to BRD4 has proliferated at rapid pace. There is compelling pre-clinical evidence from many independent laboratories demonstrating efficacy of BET bromodomain inhibitors in cell lines, as well as xenograft and genetically-engineered mouse models of hematological and solid cancers. I’ve summarized a non-exhaustive list of these studies in Figure 5. A simplified example for mechanism of action in Acute Myeloid Leukemia (AML) is shown in Figure 4, but for most cancers the underlying theme goes something like this: BRD4 disruption in cancer X results in reduced transcription of a set of Y target genes, which are important for cancer X. In some cases BRD4 is shown to be interacting (directly, or indirectly) with transcription factor Z, which is also an important player in cancer X. If you need more granularity, see the Pubmed ID’s in Figure 5, and a recent review by Shi and Vakoc. With such a vast body of pre-clinical evidence, it’s no surprise there are currently a number of start-ups and pharma companies invested in early clinical-stage BRD4 oncology programs.

BET bromodomain inhibitor (BRD4) oncology programs See Figure 6 below for a full picture of the BRD4 competitive landscape.

OncoEthix – OTX015
OncoEthix, a Swiss oncology company, is the current leader in the BET inhibitor space, with a potential first-in-class BRD4 program. OTX015 is being developed as an oral small-molecule inhibitor of BRD2/3/4, and has a similar chemical structure and in-vitro potency profile to the chemical probe JQ1 (Figure 7). This shouldn’t be surprising, since both of these molecules share the same DNA, originating from the Mitsubishi Tanabe patent literature. In fact, OncoEthix negotiated the rights for OTX015 in 2012 from Mitsubishi Tanabe Pharmaceuticals. Importantly, although OTX015 has similar binding affinity and in-vitro potency to the chemical probe JQ1, its pharmacokinetic properties are superior with a drug half-life of approximately 5 hrs.

On December 18, 2014 Merck announced the acquisition of OncoEthix for an upfront payment of $110 million with an additional $256 million in potential milestones for OTX015, an oral BET bromodomain inhibitor (see the Merck release here, and commentary from John Caroll at FierceBiotech here). This deal validates OTX015 as a promising drug candidate; more broadly, it paints BRD4 as an attractive oncology target. It’s likely that OTX015 development timelines will accelerate, and combination trials will appear as a result of the acquisition. When thinking combinations Merck’s immuno-oncology (IO) franchise would be an obvious first place to look. The scientific literature provides a basis for this approach; in some hematologic malignancies, namely AML and Multiple Myeloma (MM) there is a high level of PD-1/PD-L1 expression on tumor cells. What’s more interesting is PD-1/PD-L1 expression can increase as a response to epigenetic agents such as hyopmethylating drugs4,5. If this space is of interest to you, keep your eyes peeled for the initiation of an OTX015/pembrolizumab combination trial.
Given the deal terms outlined above, Merck clearly has faith in the early signs of activity from OTX015 in hematologic malignancies. Most recently, clinical data from OTX015 was presented in December at the ASH annual meeting (see the abstracts here and here). Additionally, interim phase I results were presented in April 2014 at AACR (view the video webcast here).

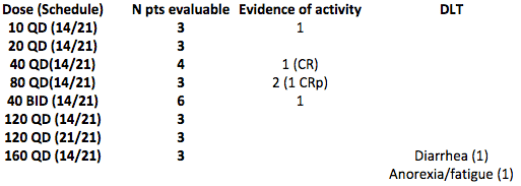
The most recent data presented at ASH was split into ‘Advanced Acute Leukemia’ or ‘Non-Leukemic Hematologic Malignancies,’ and was drawn from a single ongoing phase I trial. Both patient sets are relapsed/refractory populations, having failed two or more previous lines of therapy. Patients in the Advanced Leukemia group received OTX015 for 14 days of 21-day cycles. The median number of drug cycles was 2, with a range of 1-14+. For both patient subsets the trial followed a standard 3+3 dose escalation design. PK data demonstrated dose-proportional plasma concentrations from 10 to 120 mg QD, with trough concentrations exceeding 500 nM at the 80 mg dose group. This is a handy figure to keep in mind when comparing back to in-vitro data. For example, the GI50 reported for a hematologic cancer cell panel (~100 cell lines) ranged from ~40-6000 nM, with the mean GI50 at ~500 nM (Figure 8). Of note, the relationship between OTX015 trough plasma concentrations and GI50 is therefore different from TKIs, for example, where trough concentrations are often a multiple (e.g. 10-100X) of in-vitro GI50. The MTD was exceeded at 160 mg with reports of grade 3 diarrhea in one patient and grade 3 fatigue and anorexia in another. Anti-leukemic activity was reported in 5 AML patients at the 10, 40, and 80 mg dose levels, which included one sustained CR and one CR with incomplete platelet recovery. Two other patients (10 mg QD, 40 mg QD) had partial blast clearance, and another had gum hypertrophy resolution. See Figure 6 for a summary of the Advanced Leukemia cohort.
As per the ASH 2014 presentation, the Non-Hematologic Malignancies portion of this trial had 37 evaluable patients (18 DLBCL, 9 Other Lymphoma, and 10 MM). In this patient subset OTX015 was administered on a daily schedule for 3-week continuous cycles. The most prevalent adverse event was thrombocytopenia, which could be a consequence of the continuous dosing regimen. DLTs included thrombocytopenia, neutropenia, anemia and hemorrhage, and were found at the 80 and 120 mg dose levels. The MTD was determined to be 80 mg QD, and the recommended dose going forward is 80 mg QD on an intermittent regimen (14/21 days) to alleviate the observed thrombocytopenia and allow for platelet recovery. OTX015 exhibited meaningful activity in 6 patients: two DLBCL patients achieved CRs (120 mg QD), one DLBCL patient achieved a PR (80 mg QD), and 4 Other Lymphoma patients showed stable disease (two at 10 mg QD, 40 mg QD, 80 mg QD).my
The take home from these ASH 2014 data: OTX015 is clearly an active drug, exhibiting disease-modifying activity in relapsed/refractory AML and DLBCL. Accordingly, expansion cohorts have been triggered for AML and DLCBL to more thoroughly examine single agent efficacy. Although the numbers are still relatively small, OTX015 appears to be tolerable in these patient populations. Additionally, as a result of compelling pre-clinical data, OncoEthix is expanding OTX015 development into various solid tumors including Glioblastoma Multiforme, NUT Midline Carcinoma, Triple Negative Breast Cancer, and Castration-resistant Prostate Cancer (see Figure 6 and trial info here and here).
Other BRD4 oncology programs
It’s difficult to benchmark OTX015 because other BRD4 oncology programs do not yet have publicly disclosed data. Companies with active programs include GlaxoSmithKline (I-BET762), Tensha Therapeutics (TEN-010), Constellation Pharmaceuticals (CP-0610), and Zenith Epigenetics (ZEN-3365). See Figure 6 for related clinical trial details and other pertinent information. Early stage trials from these companies have been initiated in both solid and hematological cancers. Unlike the development path for OTX015, with GlaxoSmithKline and Tensha, the focus on solid tumors is primarily directed towards NMC. Although the true disease prevalence is unknown, NMC is thought to be incredibly rare with an estimated 20-30 new cases reported annually in the US. Widespread use of new clinical diagnostics tuned for quick and easy detection of this fusion protein may soon shed light on the exact number of patients harboring BRD4-NUT, since most laboratories lack the necessary reagents and expertise to diagnose NMC with current technologies (i.e. via immunohistochemistry and FISH). Conversely, the line-of-sight for hematologic malignancies is based on compelling pre-clinical efficacy data illustrating BRD4 dependence in these tumor types, and GlaxoSmithKline, Constellation, and Zenith have ongoing trials in this space (see Pubmed IDs in Figure 5 for further reading).
Scientists from Mitsubishi Tanabe first observed BRD4 binding activity of simple thienodiazapines6, and subsequent chemical compounds built from ‘privileged’ diazapene scaffolds have proved to be potent nanomolar inhibitors of BET bromodomain proteins. For example, the core structures of JQ1, OTX015, and I-BET762 are similar to clinical benzodiazepines such as diazepam, with a number of unique substitutions conferring binding selectivity for BET bromodomains (Figure 10). The Constellation compound, CP-0610, is chemically similar to that of JQ1, OTX015, and I-BET762, but contains an azepine scaffold instead.

Although Resverlogix is not interested in oncology indications, this public microcap Canadian biotechnology is worthy of mention when discussing the chemical structure of BET inhibitors. As a quinazolone the Resverlogix compound (RVX-208) is chemically dissimilar from the other reported BET inhibitors (Figure 10). Interestingly, RVX-208 has a selectivity bias towards the second bromodomain (BD2) of BET proteins, and lower potency than compounds built from diazapene (or similar) scaffolds7. Zenith Epigenetics, a private Canadian biotechnology company, was spun out from Resverlogix to tackle oncology indications by targeting BET proteins. Although the structure of the Zenith compound (ZEN-3365, in phase I) is undisclosed, it may be similar to RVX-208 and potentially share some of the same characteristics. If ZEN-3365 is indeed a quinazolone like RVX-208 it will be interesting to see if it can provide clinical activity similar to that of OTX015. For a more complete discussion surrounding the structural and chemical basis for targeting bromodomains see this article in Nature Reviews Drug Discovery.
Although still at the pre-clinical stage, the OncoFusion Therapeutics BRD4 program is also worthy of mention. OncoFusion Therapeutics is a start-up founded by professors at the University of Michigan Medical School. On April 28th, 2014 Medivation and Oncofusion entered into a license agreement for a number of compounds targeting BET proteins for use in oncology and other disease areas (see the Medivation release here). Through the agreement Medivation gained the exclusive worldwide rights for development and commercialization of OncoFusion BET bromodomain inhibitors. It’s unclear if a clinical candidate has been nominated yet. Although the biotech sector has seen an uptick in pre-clinical deals in recent years, this does appear to be another confident endorsement of this drug class.
Safety Concerns
Early signs of clinical efficacy are encouraging, and potentially just a glimpse into the promise of this compound class. However, a significant risk to the BRD4 thesis still lies in the safety profile of these compounds. While the remarkably broad anti-cancer activity of BRD4 inhibitors has provided much excitement, it also points to a potential liability against inflicting damage to all tissues, including those of the non-malignant kind. Unlike some other drug targets, BRD4 isn’t exclusively expressed in tumor tissue; rather, BRD4 is ubiquitously BRD4 expressed in all human tissues. Prompted by these concerns, Lowe and colleagues designed a recent study, which attempts to address safety concerns associated with BRD4 inhibition in adult tissues. They generated an inducible transgenic RNAi mouse model, which allowed for temporal BRD4 protein depletion in all mouse tissues8. Not surprisingly, depletion of BRD4 in adult mice resulted in dramatic phenotypes across multiple tissues. BRD4-depleted animals displayed epidermal hyperplasia, alopecia, suppression of normal hematopoiesis, and marked intestinal defects. Interestingly, all phenotypes were reversed through restoring normal BRD4 levels, which might suggest that unintended consequences of BRD4 inhibition could be managed through optimization of drug schedule. However, it’s not clear how predictive this model is, since many of the phenotypes observed, especially the profound intestinal defects, have not yet manifested themselves in the clinic.
Final Thoughts
Recent literature has uncovered a role for BRD4 in cancer-associated gene regulatory networks. Therefore, bromodomain inhibitors provide an opportunity to target misregulated transcriptional programs in cancer. The vast array of pre-clinical data generated thus far provides a compelling basis to move into human trials across a number of different indications. While current BET inhibitors target BRD2/3/4, it may be beneficial to design more specific inhibitors for BRD4, and eventually develop chemical tools that allow discrimination between the disease-relevant functions of each bromodomain present in BRD4 (i.e. BD1 vs. BD2). However, a high level of protein identity among BET proteins may ultimately preclude development of more selective BRD4 inhibitors. Continued research efforts aimed at examining disease-relevant BRD4 protein-protein interactions, genomic binding sites, and downstream transcriptional effects are likely to uncover novel cancer-specific vulnerabilities, and potentially inform future drug discovery efforts. It will be exciting to watch the development path of this drug class as new indications are explored and trials progress towards larger efficacy studies.
References
- French CA. Pathogenesis of NUT midline carcinoma. Annual review of pathology. 2012;7(247-65.
- Filippakopoulos P, Qi J, Picaud S, Shen Y, Smith WB, Fedorov O, Morse EM, Keates T, Hickman TT, Felletar I, et al. Selective inhibition of BET bromodomains. Nature. 2010;468(7327):1067-73.
- Nicodeme E, Jeffrey KL, Schaefer U, Beinke S, Dewell S, Chung CW, Chandwani R, Marazzi I, Wilson P, Coste H, et al. Suppression of inflammation by a synthetic histone mimic. Nature. 2010;468(7327):1119-23.
- Atanackovic D, Luetkens T, and Kroger N. Coinhibitory molecule PD-1 as a potential target for the immunotherapy of multiple myeloma. Leukemia. 2014;28(5):993-1000.
- Yang H, Bueso-Ramos C, DiNardo C, Estecio MR, Davanlou M, Geng QR, Fang Z, Nguyen M, Pierce S, Wei Y, et al. Expression of PD-L1, PD-L2, PD-1 and CTLA4 in myelodysplastic syndromes is enhanced by treatment with hypomethylating agents. Leukemia. 2014;28(6):1280-8.
- Miyoshi, S., Ooike, S., Iwata, K., Hikawa, H. & Sugaraha, K. Antitumor agent. International Patent No. PCT/JP2008/073864 (WO/2009/084693) (2009).
- Picaud S, Wells C, Felletar I, Brotherton D, Martin S, Savitsky P, Diez-Dacal B, Philpott M, Bountra C, Lingard H, et al. RVX-208, an inhibitor of BET transcriptional regulators with selectivity for the second bromodomain. Proceedings of the National Academy of Sciences of the United States of America. 2013;110(49):19754-9.
- Bolden JE, Tasdemir N, Dow LE, van Es JH, Wilkinson JE, Zhao Z, Clevers H, and Lowe SW. Inducible in vivo silencing of Brd4 identifies potential toxicities of sustained BET protein inhibition. Cell reports. 2014;8(6):1919-29.
Disclaimer: All opinions expressed on Oncology Discovery are my own and do not necessarily represent the position of my employer. The information presented within this article is not a solicitation for investment.
Copyright © 2015 Oncology Discovery. All Rights Reserved. Unauthorized use and/or duplication of this material without permission is strictly prohibited.

Comments are closed.